In the June issue of Health Affairs a study was published discussing ACO’s and the rise in physician leadership within the organizations. One of the goals of the Affordable Care Act was to hold physicians more responsible for the care of their patients, by rewarding healthcare providers for improving the quality of care and lowering healthcare costs, the ACO model was born. Slow to start, ACOs have no risen in popularity, with more than 600 Accountable Care Organizations operating throughout the U.S.
“What is an ACO? — An ACO is an accountable care organization made up of doctors, medical groups, hospitals, and other healthcare professionals who work together to deliver high-quality, coordinated care to the patients they serve.”
There are many various types of ACOs, some are made up of solely primary care providers, others include a variety of specialists and others encompass hospitals and post-acute care providers. However, the study showed that physician-led structures seem to be operating best, meaning they are more likely to have complete care management programs, advanced IT programs and the most satisfied patients.
Former CMS Administrator, Dr. Mark McClellan attributes this to physicians’ personal experience and ability to identify areas for improvement firsthand and measure the impact of their efforts. The Director of the Dartmouth Institute and co-author of this study, Elliott Fisher, MD, MPH stated, “Physicians’ buy-in the payment reform is likely to be critical to the success of the health care reform.” He continued to say; “The findings suggest that physicians are taking seriously their responsibility to lead change in the health care system on behalf of their patients.”
It is certainly pleasing to know that physicians are in support of these changes and are taking on the responsibility of helping to ensure the betterment of care for their patients. As more ACOs are brought together, this report will help providers determine if the path is right for them and consider which structure is best.
To read more about how ACOs originated and to view statistics on the success some organizations have found, check out the Health Affairs blog here: http://healthaffairs.org/blog/2014/05/30/aco-results-what-we-know-so-far/

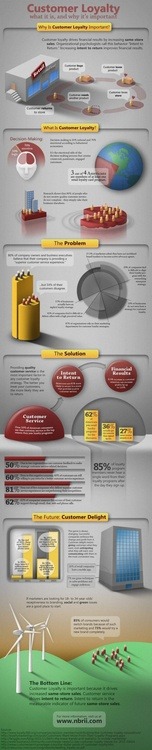 (See image here:
(See image here: