The RBMA Building Better Marketing Conference in Long Beach, California went off without a hitch earlier this week, bringing together the best radiology professionals from all across the world. On Sunday evening, the attendees mingled in the lobby of the Renaissance Long Beach hotel meeting new friends and reminiscing with the old. With the sound of an acoustic guitar in the background and the sea breeze filtering through the open doors, everyone knew we had arrived in Cali baby.
Monday morning is hard for everyone, but Terri Langhans opening presentation got everyone’s gears going for the week. She asked us, “How do you stand out in an industry where everyone looks alike?” By comparing the radiology industry to the airline industry she led us to see the opportunities available to make ourselves stand out. Think about the differences in flying Southwest versus Delta, even just the comedic way Southwest delivers their safety information. “You don’t have to be a comedian, you just have to have a personality,” Langhans quoted. Her message was to make sure we do small things with character, because the more similar you are, the more your differences matter.
In radiology, each touch point your patients have with your center matters. A touch point is any point of contact, for instance; phone trees, parking, welcomers, front desk employees, techs, radiologists, schedulers, even your billing department. Langhans’ message essentially, is that your touch points should be talking points, or components that set you apart from the competition and contribute to a strong culture for your organization.
(Check out photos from the event on the RBMA Facebook Page here: https://www.facebook.com/RBMAConnect)
The schedule over the next two days was packed full of sessions covering content including:
- Writing creative marketing/web content
- Social media for radiology providers
- Stark Law and Sunshine Act
- Advancements in breast imaging
- Search engine optimization
- Selecting and utilizing a CRM
- Rebranding techniques
- Using referral metrics to drive business
- Finding an “Open Table” model for radiology scheduling
- Interventional radiology practice development
- Imaging market changes and opportunities
- Content marketing strategies
- Customer service and efficiency
- Campaign creation versus ads
- Benchmarking for marketing and sales
- Quality initiatives for independent hospital-based physicians
- Advice for IDTFs competing with hospital systems
In addition to those very focused sessions, conference attendees gathered together for roundtables discussing marketing efforts they have used that were effective and the industry issues that have been keeping them up at night. Tuesday morning was also kicked off by a 5 Minute Forecast from a panel of RBMA experts. All of whom were geniuses; well spoken and wonderful. (Cough, cough… this is shameless brag, as I was one of them.) After the forecasts, which predicted increases in patient-consumerism, market transparency and the increased weight of strong industry relationships, the floor was opened up to the attendees and they were given the chance to ask any marketing questions they had up their sleeves. The session, entitled “Stump The Marketers,” was my favorite part of the entire conference because it enabled us to engage in candid conversation about the real issues we all face on a daily basis. Topics covered included:
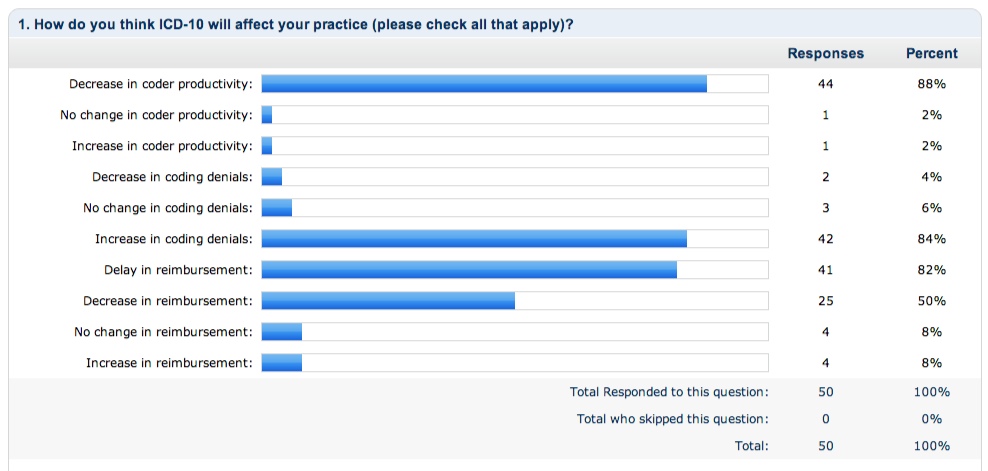
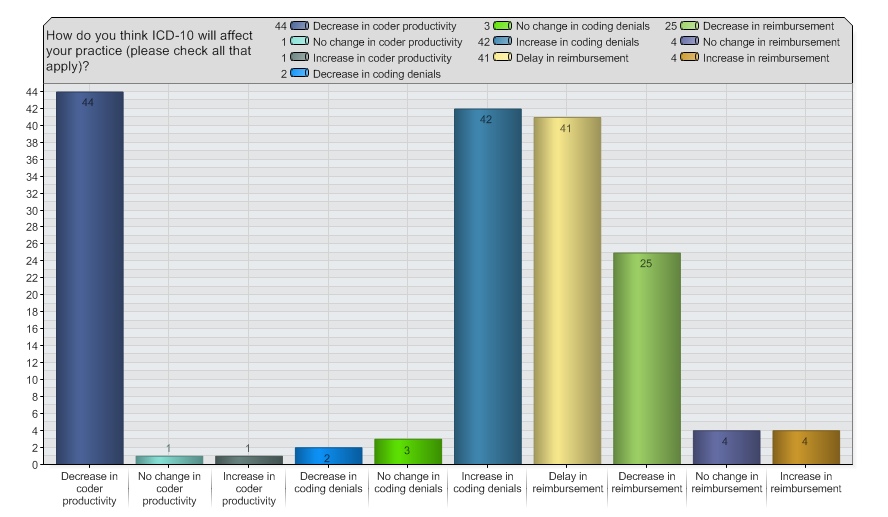
- ICD-10 and the effect on marketing representatives: It was determined that the coding changes will give marketers a chance to stand out as early adopters and even give training opportunities to their referring offices.
- Direct targeting and re-targeting campaigns for patients: Some wondered if this form of internet marketing could be considered invasive, but we decided that if the patient is already interested in you, they will perceive you in that way.
- Utilizing technology for patient communication: We decided that nothing can be replaced by one-on-one communication and people do not want to be made more convenient. If a patient ops in for email or text reminders or event updates, that is another opportunity.
- Spending money on traditional marketing and advertising like the phonebook: These historically expensive methods have no way of being measured as far as ROI goes, so most marketing pros have started to turn towards internet marketing instead.
Anyone that was a part of the conference will say that they learned a lot and will remember fondly how great the smartphone application was (especially with the neck-in-neck race between Erik W. and Brenda B. for top users), the great bartenders at "Sip", the great elevator struggle of 2014, the California-themed Quest Awards and how wonderful the RBMA faculty was for organizing such a spectacular event.
Overall the conference was a huge success. The RBMA team certainly knows what they are doing and each year the content and sessions get better and better. We are already looking forward to next year’s event, it is going to be in Nawlins’ after all! Until next year everyone, can’t wait to see what all we will accomplish in 2014.